We arrived at Edinburgh’s Western General hospital. I only sat down in the waiting reception for a couple of minutes and a nurse came with a chariot to take me to a bed and get me clarked in. One of the consultants gave me a thorough going over. Well the question is, how long are we keeping you? She asks. Steve prompts a reply well anything less that five weeks is a bonus, but it would be a preference to have her home for Christmas to share a Brussel sprout or two 😀 The consultant broke into a smile and said. No promises but be will do our best. Within an hour and a half I had been booked in, blood taken , urine sample given, cannula inserted, porter called and I was now getting wheeled along to the ward.
I get into the ward of four, the nurse helps me out of the wheelchair, and assists me into the bed. She points out where the toilet and shower room is. After explaining everything to me, she placed the buzzer close to me and said if you need anything press the orange button, and we will come to you. I thanked her. Steve put my things in my locker, spoke to the nurses, and then came back to see me, gave me a kiss and hug and headed off home – for Steve it had been a long day. I looked round the room. In the bed opposite the lady was sound asleep propped up with several pillows, the bed next to her, the lady was awake, hello I’m Jess she calls over to me. The bed next to me has an elderly lady who informs me she is going home in the morning. She seems so happy about it. All in all three elderly ladies, a quiet room, an exhausted me, hopefully I will get a sleep.
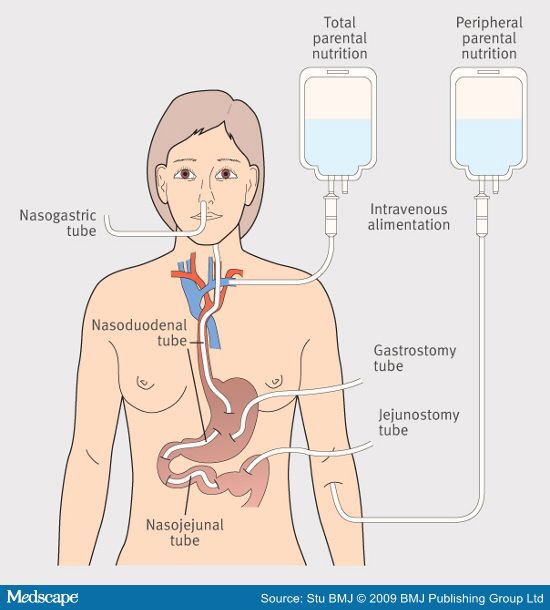
I did sleep, the staff were brilliant and the room mates friendly. The lady went home and we got a new patient. Jess and I talked away like a couple of school kids, we laughed and joked and had so much in common – I’m 49 and Jess is 87 years of age. Anne the lady opposite me was very deaf. It made conversation difficult. My consultant came to see me and it was decided no food was to be taken orally, the only fluid was when I was taking my medication. And it was to be minimal water when taking meds. The lack of oral fluid takes a wee bit of getting used to. Your mouth feels perched. Your lips press together tight. The nurses are very kind and supply you with endless nice cubes and foam lollies, you can clean, rub your mouth and or throat. It really does help. Mouth wash helps too. The dietician came too and the plan was to continue feeding through the pej at 100 mls per hour for 20 hours out of every 24 hours.
Consultant visited next day – we chatted. Talked about how we thought the hole may seal up. I told her about us watching supervet, the honey helping the cat. My dedicated husband digging out honey out of the cupboard and unfortunately how unlike the cats jaw repaired fairly quickly my tummy was sticky and clothes sticking to me. She looked at me and said Elizabeth what were you doing with the honey? I laughed I explained Steve spread it on a half slice of toast and it leaked out as soon as it was in. Thank goodness for that she said. I guess she watched supervet. He actually rubbed the honey on the cats wound. I think she had visions of us rubbing the honey on my tummy – no such luck – ha ha ❤️
The nurse came to do my flush on my pej. Oh boy was it difficult to flush. It actually took 15 minutes to get 50mls of sterile water though the syringe. The tube is so fine. Attached to my tummy is my pej and then my feeding pump. When I get my 4 hours of, this is when I want to shower. I am still attached to the dextrose drip – for the fear of having a hypo on their watch. But after being on TPN ive mastered being able to shower with such gadgets. Once the flush is done. I prepare myself for my expedition. The walk to the toilet is still a difficult one – I do it in a couple of trips, trot along carrying two towels and using the drip stand as an aid – made the first trip to the shower room. Now I will head back and get my clean pjs and toilet bag. As I turn round, the nurse is standing there with my things. Don’t you try and do all that on your own, we are always here to help , she said. Got to admit I was so glad she brought them. Now are you going to be ok? the nurse asked. I nodded. I put down my clean pjs on the chair, and started taking what I needed out of the toilet bag. I did the needful, managed somehow to get my clean pjs on. As I was about to put my socks on I could feel the beads of sweat running down my back, I eased myself up from the chair, and decided to walk back to the bed as I was. I really needed to lie down. As I was walking over to my bed the nurse came and took my toiletries from me, put them on my locker and then quickly walked back and took my arm, my you are very flushed she said. Oh it’s the heat of the shower, I just need to lie down a minute. I said. She walked me back to my bed, helped me back into bed. I was so grateful. That shower had just sapped me of all the energy I had conserved in my body. Half an hours rest and then it was time to get my feed back up and running.
A young man walks into our room, now ladies who would like to put a request on the hospital radio tonight. I’ve been in hospital many many times – in fact I wouldn’t like to think how many hospital admissions I’ve had, and I personally have never listened to hospital radio. Due to Anne’s deafness she didn’t take part, however the rest of us all requested something. His parting words were have a go at our competitions. Makes the evening fun.
Teatime came – the three ladies had their meal . I stayed attached to my feed. My body must be fed – my tummy doesn’t even rumble. They had fruit crumble for pudding – one of my favourites. It must have sent messages to my brain and got my gastric juices working overtime; when it was time fir a dressing change my tummy had been excreting gastric juices that resembled PVA glue – just the kind that it makes up on its own. My brain must have been saying to the belly ha ha doesn’t this food look good, smell lovely. That old saying my belly thought my throat had been cut but instead of rumbling grumbling noises I get leaking discharge. Then visiting – which I always enjoy when my hubby comes in to see me. I get a chance to see how he is, and catch up with the outside world. Visiting finished at 8pm.
8pm was the time the radio show started. The three of us put our headphones on. The music played, the dj chatted – we bletherered over it. Competition Time. It was a mystery voice, we listened, the lady, Avril, in the next bed said its Chris Evans. I shouted out the telephone number to her, she dialled it in her phone, hey presto its ringing she says. Oh my goodness I’ve won. She says, i have never won anything in my life. That boost fair cheered us up. We listen some more and sing along , the DJ tells us another competition is coming up shortly: this time sport. The question is how many people watched the Fifa World Cup world wide in 2006. There are three options. I’ve heard this question before. I know I have, the answer 26.29 billion jumped out at me. I shouted out the answer. Jess said phone. I picked up my mobile and dialed the hospital radio number. Engaged tone. Try again. Jess shouts over. I try – beep beep: rather than a melodic ringtone. The music stops on the radio, that’s it, the dj will announce a winner I’ve resigned myself to defeat. The dj’s cheery voice makes you smile, he introduces a chap called Gary on the line. Gary is calling from The Edinburgh Royal Infirmary. He is asking for a request. The DJ then mentions the completion. Oh I’m no good with mystery voices. He says. It’s ok Gary, Avril won that competition, we are onto a new one. He asks the question again. I’m not sure says Gary, but at least I can just guess A, B or C. At this stage I’ve got steam coming out of my ears. My competitive streak wanted him to get it wrong so I could phone in. He answers. Oh sorry Gary, that’s the wrong answer. Both ladies and the nurse that was in our room at the time cheer. I phone again. It’s still engaged, I look up, both ladies in chorus – keep trying. So I do. Finally it’s ringing. He asks me the question. And yes I get it right. Competition winners receive borders biscuits. My reward was different and I was pleased with what I won. A mug and a key ring.

All that excitement had tired me out. It was 10pm. Time for the late night drug round. The nurse came round and did all our meds. The other nurse did our obs and then it was time for my next feed. The familiar beeping of the pump to let me know the feed was finished and time to change. The nurse came to detach the finished feed bottle, flush the tube, check the peg site and then restart a new feed for overnight feeding. The nurse came armed with a syringe, and sterilised water. She drew up water in the syringe. Carefully attached it to the appropriate part of the peg and pushed to get water into the tube. We looked at each other. The syringe was locked tight. It wasn’t budging a cm. she tried to push harder. Nothing. Her face was rosy pink. This isn’t budging. Does it ever get like this.? She asked me if it often gets like this. I answered with its frequently difficult to push but never as hard as this and I’ve never not been able to put water through the tube. The extension is a very fine tube and much longer than the original gastrostomy. I think I need some help here. She said. We abondoned the feed. She paged the on call doctor, since it was now 11.50pm. The duty doctor came. It wasn’t budging for them either. A decision was made for the night. A dextrose drip would go up to maintain my blood sugar levels and a GI consultant would come see me first thing in the morning to do something with the blocked tube. And overnight the nurse would regularly check my blood sugar levels with the finger pricker to make sure the drip is doing its job. It did.
8.30am – the GI consultant was standing at the bottom of my bed. Well trouble what are we going to do with you now He said in his thick Irish accent. I grinned at him and replied unblock this tube if you know what’s good for you! He drew the curtains round the bed. Then got the syringe and attached it to the tube. He wiggled and pumped back and forth. Nothing. He detached the syringe. He then pulled the tube slightly back, I could feel a strange feeling in the pit of my stomach. Oh that’s a tad sore I say. Yes you’ve gone a whiter shade of pale was his reply. Just bare with me, please, ive got a plan he continues to say. So I lie there and wait in hope. He pours sterile water into a beaker then draws it up in the syringe. He attempts to push some into the tube, it’s still not moving. He uses the push pull method once again and then all of a sudden WHOOSH!!!! Me and my bed are wet. Water and gastric contents on pjs, face, hair, and bed linen. The doctor tries to apologise. While laughing I’m thanking him for unblocking the tube. Im so relieved. And much more comfortable. The nurse joins us and starts cleaning me up. The doctor leaves us and goes attend to something else. Half an hour later I’m in clean fat face pjs, got the hospital bed propped with pillows my blankets, iPad, writing material. Looks like I’m all set for lying on a sun lounger by the pool in Ibiza not getting ready to try a feed. The blue curtain round my bed slowly moves, a voice quietly asks, is it safe to come in Elizabeth? It was the doctor who just unblocked my tube. However, he was more concerned with drenching me and the bed. I tried to put on a grumpy stern face and say I was annoyed. I couldn’t. Soon as I saw him. We both laughed. Let’s try the feed then he said. And so we did. It worked. For two days,
For two days all I had was feed via the gastrostomy tube. The only thing that went down my throat was my medication. On day three the tube blocked again. This time there was no flushing it. I’ve got to admit it was getting scary. The consultant explained he couldn’t push too hard with the syringe for the fear of the tube explicating. That statement terrified me. There is only one thing to do – take the jejunostomy tube out. Once he had actually said the words – take it OUT. I wanted it removed NOW. So I got my way. It was removed while I was in my hospital bed in the ward. Got to say it was a strange sensation. There was a slight tugging feeling. Then my tummy felt like it had never before: the doctor carefully pulled the tube at a slow steady pace. This wasn’t an experience I was comfortable with. I lay still and thought it best to co-operate in any way I could. My whirlwind tornado tummy had died down. As he continued to pull the tube gently, gungie watery gastric juices ran out as the tube was easing out. Then there was a click. At last the end of the extension tube. That was it out. Thank goodness. Doctor and patient both relieved.
Time to Take the big step back to straight forward gastrostomy feeding (peg) . Sort the feeding regime with the dietician. Start of on a very slow rate with my pump. Just 20mls per hour for 5 hours. Remember I haven’t been fed direct into my tummy and how much am I going to leak. Five hours later – dry dressing. I felt like a toddler that had gone all night without peeing the bed. The nurse came to flush my tube and check everything is ok before increasing the rate. And so the rate was increased gradually over the next 24 hours until I reached 80 mls per hour. At this rate there is a leak when the feed goes in, but only a slight leak. I asked the consultant when the hole would seal up and I would stop leaking his answer was how long is a piece of string. I just don’t heal as well as some people. And take much longer than others.
- We had a discussion at the hospital and decided I could go home on my feeding regime with
- The support of my district nurses coming in through the week to do my dressing, check the tube in general, deal with my skin, give me my lanreotide injection, and any other general medical/physical/emotional support they always do
- Community dietician coming to the house very regularly to check on feeding regime, change my prescription if need be. Give instruction on changing connectors for tube. Take my weight. Give us general support.
- Regular contact with my GP.
- Home support from my hubby, and boy do I get this ❤️
Well the staff at the hospital had been tremendous, my room mates were great company for a bunch of sick folk. I even managed to get some online Christmas shopping done – I bought a couple of bits and bobs or Steve, Tony and Stuart. But I’ve got to admit I was ecstatic that I was leaving them. The thought of Our own sofa with my Steve, Buddy and Bella was just what the doctor ordered. I yearned for my home life back.
55.923618
-2.865043